Fact: the actual “balance of estrogen” is important when we talk about reproductive health and effects on fertility; more than the level of one estrogen or the other. In order to achieve system-wide hormonal balance, you need to know about estrogen, how it is metabolized by the body (estrogen metabolism), and how to keep it balanced with other hormones related to your reproductive wellness.
Estrogen dominance, or increased estrogen relative to progesterone levels (or to testosterone levels in men), is a big problem in the modern world for many reasons. Estrogen production can be greater for certain individuals (those who are obese for example), there can be problems with the way estrogen is metabolized, and there can be an increased intake of xenoestrogens (which are external forms of estrogen mimickers or foreign estrogens)—all of which can contribute to estrogen dominance.

Estrogen Science You Need to Know
There are three types of natural estrogens in the body:
- Estrone or E1 is the type of estrogen predominant in the body after menopause.
- Estradiol or E2 is a particularly strong form of estrogen that the ovaries make during the reproductive years.
- Estriol or E3 is a weak form of estrogen seen in the body mainly during pregnancy.
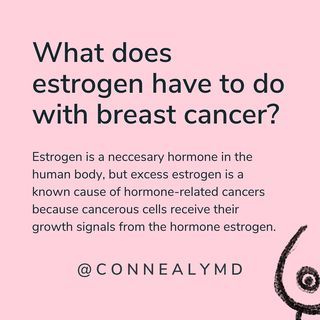
There are two estrogen receptors (binding proteins) in the body; alpha and beta receptors. Alpha receptors promote the growth of cells and beta receptors block cell growth. Estriol binds to alpha receptors, while estradiol binds to both alpha and beta receptors. Estriol blocks cell growth because it primarily binds to the beta receptors.
Estrogen metabolism:
Estrogen needs to be broken down when it is no longer needed. There are two pathways to estrogen breakdown. The first leads to 2-hydroxyestrone and the second leads to 16-hydroxyestrone. It turns out that 2-hydroxyestrone is healthy for you because it blocks the type of estrogen that can possibly lead to certain reproductive cancers. On the other hand, 16-hydroxyestrone is inflammatory and is linked to high levels of omega-6 fatty acids, low thyroid conditions, obesity, and toxicity from pesticides. Too much 16-hydroxyestrogen has been associated with lupus, other autoimmune diseases, and breast cancer.
The Risks of Estrogen Dominance
Estrogen dominance or “too much estrogen” has been linked to many health problems. Exactly why there is so much estrogen dominance in developed countries lately isn’t known but it certainly can be related to our diet, exposures to pesticides or herbicides, and the presence of xenoestrogens in products we use every day & our stress load. Estrogen dominance is a problem facing men and women alike.
Estrogen dominance in women is associated with many possible symptoms. These include the following:
| Menstrual irregularities Fibrocystic breast disease PMS symptoms Decreased libido Headaches Emotional symptoms like anxiety, insomnia, brain fog, and depressionPCOS | Endometriosis Weight gain and obesity Reproductive cancers like breast and uterine cancer Benign uterine fibroids Nodules of the thyroid gland Vaginal discharge with odor |
Men can have issues with estrogen dominance as well. Things men might experience include breast enlargement, infertility, erectile dysfunction, and prostate cancer.
Controlling Estrogen Metabolism With Diet
Too often people jump right to hormonal treatments when we should take a step back and work to restore function within the body. In cases where estrogen dominance has caused serious conditions such as endometriosis, these recommendations will help improve symptoms, but the root cause must be assessed & addressed to allow the body to heal.
The goal of managing estrogen in your body is to make sure you don’t eat too much in your diet, don’t get exposed to foreign estrogens or “xenoestrogens”, and promote the breakdown of estrogen in a healthier way. As you can imagine, it is better to metabolize estrogen so you have more protective 2-hydroxyestrone than 16-hydroxyestrone.
There are things you can do to shift your estrogen metabolism toward having more 2-hydroxyestrone made as a metabolite. These are a few measures you can take:
- Eat more cruciferous vegetables like broccoli, turnip greens, Bok choy, wasabi, Brussels sprouts, kale, cabbage, greens, and cauliflower, which are high in indole-3-carbinol and diindolylmethane (DIM) that help regulate estrogen metabolism.
- Consume more omega-3 fatty acids that you find in fish (wild caught) like salmon, sardines and cod liver oil, cage-free eggs, avocado, nuts, and flaxseed products.
- Eat foods high in vitamin B6, vitamin B12, and folate.
- Lose weight and exercise more. The fat in your body stores excess estrogen, contributing to estrogen dominance.
- Consume prebiotic and probiotic foods to help rebalance your gut microorganisms, having a big effect on estrogen balance in the rest of the body.
- Reduce stress, because this can increase cortisol levels, offsetting the balance of estrogen and progesterone in your body.
- If you eat meat, choose organic, grass-fed meats and dairy products, which are free of the hormones fed to non-organically raised beef.
- Try anti-inflammatory plant-based herbs like Turmeric (Curcuma longa) and Ginger (Zingiber officinale).
- Eat a lot of fiber in your diet, which will decrease estrogen absorption in the food you eat and will increase fecal estrogen excretion.
- Decrease alcohol intake because alcohol can block estrogen metabolism and will increase the body’s estradiol levels.
- Think about supplements that restore estrogen balance, such as DIM (diindolylmethane), Maca (Lepidium meyenii), Milk Thistle (Silybum marianum), Passionflower (Passiflora incarnata), Rosemary (Rosmarinus officinalis), and alpha lipoic acid.
Look at your lifestyle too:
- Avoid xenoestrogens, which can be found in products containing BPA (bisphenol A), PCBs (polychlorinated bisphenols), and phthalates (found in plastics, plasticizers, and other products).
- Stay away from hormonal birth control methods & HRT, as these are high in estrogen and will contribute to estrogen/progesterone imbalance.
To Sum It Up
Your goal: Consume healthy whole foods and to change your lifestyle so you can metabolize the estrogen you have in your body naturally in healthier ways. There are things you can do to tip the balance toward better estrogen metabolism, leading to fewer side effects from estrogen dominance. Finally, avoid the nasty xenoestrogens, which mimic estrogens in your body in the unhealthiest of ways, contributing to the overall problem of estrogen imbalance.
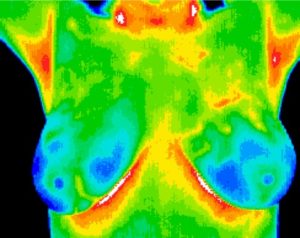
Consider Breast Thermography, to assess the impact estrogen is having on your breast health. There can be 50 times more estrogen stored in the breast tissue, then will ever be be found by testing blood, urine or saliva.