Breast Thermography is a non-invasive and painless test, with no radiation involved. It can detect and monitor early warning signs of breast dysfunction and inflammation.
This type of breast cancer screening is particularly useful for people under the age of 50. This is because mammography, another type of screening, can be less effective for this group.
Thermography is approved by the FDA since 1982 for use a s an adjunct to to mammography. and .
How Thermography works

Thermography, also known as thermal imaging, detects the rise in skin temperature which may occur when cancer cells are multiplying.
The way Thermography, or thermal imaging, works is based on how cancer cells grow. When cancer cells are growing and multiplying in a tumor, blood flow is very fast in that area.
Increased blood flow makes skin temperature increase. This rise in skin temperature is what breast thermography is aiming to detect.
There is a debate among doctors about how useful Thermography is as a way to diagnose breast cancer. The American Cancer Society have said that it will take time to see if it is better than, or equal to, current tests.
Process of a Thermograph
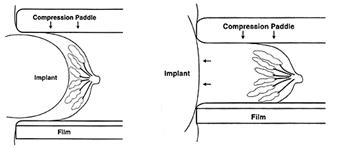
Breast Thermography is a non-invasive physical test.. It is also “non-compressive,” which means that it does not put force on, or squeeze, the breast, as is the case with breast mammography exams.
Some people are worried about the force put on breasts in a mammogram, so prefer the idea of a Thermogram.
Thermography uses digital infrared imaging to detect subtle changes in the breast based on symmetry. It looks for clear abnormalities in one breast in comparison to the other. This has to be adjusted when using on individuals who have undergone a mastectomy
To understand a Thermography report, it is necessary to know two things about cancerous breast tissue, compared to normal breast tissue. These are:
- there is more metabolic activity (biochemical reactions)
- there is increased blood flow
These aspects of breast cancer tissue result from the cancer cells doing all they can to maintain and grow. Another side effect of this is a rise in skin temperature.
Ultra sensitive cameras and computers can detect this increase in temperature. They produce high-resolution images.
Using thermography with other tests

T
Thermography can be used alongside other tests, such as mammographic or ultrasound screening.
Normally if a Thermograph alone is used, the images taken will be kept on record and used for future evaluations. The idea is that an initial Breast Thermography Test, which can be used on people as young as 18, will provide a baseline.
Future tests can then be compared to this baseline to see if there are any changes or abnormalities that develop.
Follow up tests
If abnormalities are detected, then follow-up procedures will be required to investigate further. This may include a mammogram.
These follow-ups can also rule cancer out, as the images could be showing a host of other breast diseases. When abnormalities are present it could be a sign of:
- cancer
- fibrocystic disease
- infection
- vascular disease
Results categories
After the test, the reports are divided into five categories. These is known as the TH (thermobiological) grading system. The categories are as follows:
- TH-1: Symmetrical, bilateral, nonvascular (non-suspicious, normal study)
- TH-2: Symmetrical, bilateral, vascular (non-suspicious, normal study)
- TH-3: Equivocal (low index of suspicion)
- TH-4: Abnormal (moderate index of suspicion)
- TH-5: Highly abnormal (high index of suspicion)
Follow-up exams are needed at different times for each category, a rough guide is as follows:
- TH-1 and TH-2: every year
- TH-2: every year
- TH-3: every 6 months
- TH-4 and TH-5: every 3 months
Effectiveness
People do not have to decide between breast thermography or mammography, but may use them both. Using the two together can be more effective.
The use of Thermography, Mammography, and a clinical exam is known as the “multimodal approach”. Using this approach can help identify around 95 percent of early stage cancers.
Technology

Thermography uses sophisticated cameras and computers to capture infrared photographs.
Thermal imaging technicians capture an infrared photograph, or heat image, of the breast.
This can then be printed in high resolution for a doctor to study, or may be sent to them electronically.
History
Thermography has been experimented with in medical science for many hundreds of years. However, it wasn’t until 1972 that the Department of Health, Education and Welfare announced that Thermography was “beyond experimental.”
This announcement applied to the use of the technology for many areas, including the evaluation of the breast. The advance in technology since then has seen Thermography become recognized in multiple areas of medicine, including breast health.
Heat patterns
The cameras used in Breast Thermography produce ultra-sensitive, high-resolution infrared images. These images show heat patterns and identify changes in the temperature of the skin and blood flow.
Many other technologies that test for breast cancer work in other ways that do not involve looking for heat patterns. These tests include:
- mammography
- ultrasound
- MRI scans
- X-rays
Breast thermal risk index
Other factors can affect the results of a Breast Thermography. So, often doctors will use the Breast Thermal Risk Index to help ensure more accurate results. This includes:
- age of person
- family history of breast cancer
- medication, including birth control and hormone pills
- menopause
- if the person is overweight
Benefits
Thermography offers the opportunity for early detection of breast cancer and has a number of specific benefits.
Earliest possible detection
A Thermogram enables abnormalities to be detected sooner than other procedures.
Compared with other procedures being used on their own, Thermography makes it possible for cancer or pre-cancerous growth to be detected up to 10 years sooner than they may otherwise have been.
Close monitoring
Thermography means that people at potential risk of developing breast cancer can be monitored closely.
Outlook
If breast cancer is caught at an early stage through the use of thermographs, this increases a person’s treatment options and should ultimately lead to a more positive outlook.
However, Breast Thermography only has the potential to identify early warning signs. Thermography, mammography and ultra sound cannot diagnose breast cancer, Only a biopsy can do that, Thermography is the only assessment tool that may highlight a potential problem years before a lump is detected on other structural tests. Thermography is truly about Breast cancer Prevention, a health and wellness Programme can be followed to restore Breast Health. Again the use of Thermography will identify the effectiveness of such a programme.
<